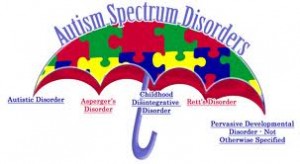
I was reminded again this week how much I enjoy working with adults with Asperger’s or autism. I frequently work with children on the autistic spectrum and help guide them and their parents through the maze of nutritional factors and concerns that either affect autism or are affected by it. With kids the reasons for nutrition therapy often revolve around identifying food sensitivities which affect behavior and/or gastrointestinal disorders, nutrition deficiencies, limited food choices, food/medication interactions, and/or concerns about poor growth. I enjoy working with this population because there is such a multitude of variables to consider, and because I can empathize with the parents who often have a history of dealing with practitioners who just don’t “get” their kids and how they don’t fit the mold. Standard recommendations often don’t work with these kids. Sensory issues, difficulties with change and transitions, and communication challenges all need to be taken into account…all while working to unravel the mysteries of what nutritional factors will have the greatest impact on the child’s health and well-being. As always, I like a good challenge. And I must admit that I also enjoy using my own tendencies to “think outside of the box” to help families find creative solutions to eating challenges.
I have had the privilege of working with several young adults on the autistic spectrum as well. They really are some of my favorite patients. Since Asperger’s didn’t even have a name until 1994, many adult’s with Asperger’s lack the advantage of having had the multiple therapies that the young people have access to today. Many are also unaware that they have tendencies that are common to people on the autistic spectrum. Professionals who are used to working with individuals with autism can help them to identify some of these traits and strategize how to deal with them. My adult patients with Autistic Spectrum Disorders (ASD) come to me with a variety of concerns, most of which are similar to those that the general public seek nutrition therapy for. I’ve coached adults athletes with ASD, and helped others with concerns about high cholesterol, nutritional deficiencies, eating disorders, and weight management – to name a few. The overall objectives for nutrition therapy are the same as with the general public, but the approach must be tailored to accommodate individual food jags, sensory issues (texture, temperature, etc.), available resources, organizational style, temperament, and capacity to tolerate change/transitions. Too much, too fast is often a deal-breaker. Assessing medical or sports performance needs must be ac companied by assessing psychological, intellectual, and neurological needs and tolerances…and I can guarantee you that these vary greatly amongst adults with ASD. My joy comes in being able to work with individuals to step back and look at the big picture. This includes identifying what needs to happen to meet health and fitness goals, the potential obstacles, and helpful factors. From there we construct individual nutrition plans and goals aimed at helping individuals to be successful – often a few steps at a time. Understanding that differences don’t always equal flaws, and listening carefully to understand systems that are helpful for individuals with ASD are key to designing successful nutrition plans for this fabulous population. I love being able to “think outside of the box” and appreciate differences instead of fighting them. Adults on the autistic spectrum have a variety of challenges to deal with, having to work with a rigid nutrition plan doesn’t have to be one of them.
companied by assessing psychological, intellectual, and neurological needs and tolerances…and I can guarantee you that these vary greatly amongst adults with ASD. My joy comes in being able to work with individuals to step back and look at the big picture. This includes identifying what needs to happen to meet health and fitness goals, the potential obstacles, and helpful factors. From there we construct individual nutrition plans and goals aimed at helping individuals to be successful – often a few steps at a time. Understanding that differences don’t always equal flaws, and listening carefully to understand systems that are helpful for individuals with ASD are key to designing successful nutrition plans for this fabulous population. I love being able to “think outside of the box” and appreciate differences instead of fighting them. Adults on the autistic spectrum have a variety of challenges to deal with, having to work with a rigid nutrition plan doesn’t have to be one of them.


I have some questions. Have you had experience in outling dietary programs for adults with Autism. My brother is in a group home and for at least the traditional reasons for having a better diet would benefit. I can’t help but be hopeful that a fully nutrient dense diet wouldnt’ at least help him better relax and deal with transitions large and small easier.
I haven’t found a lot of writing describing great improvements among the adults with “classic” symptomolgy of which my brother is a textbook guy.
I run into roadblocks from my mother, a senior, who is believes we will never get the director of his group home on board. How would we proceed with three other residents. Where do we start? etc. etc.
I feel that we start with his PCP and get prescriptions for blood tests and dive in with a nutrient dense diet. Replacing one food with the next. I follow a nutrient dense diet albeit without the same challenges an person with autism has but notable my body embraced the introduction of abundant green foods quickly. With direction from a nutritionist and hopefully guidance from a spcialist in this field my brother can enjoy a more comfortable life. At the very least to be less plagued by anxiety and allergies would be a great step.
Thank you,
Susan O’Donnell